When tendons are repeatedly placed under more tension than they can deal with, they can have a failed healing response. This can cause changes to the structure of the tendon and is known as a tendinopathy. When this occurs in the tendons of the gluteal muscles it is referred to as gluteal tendinopathy.
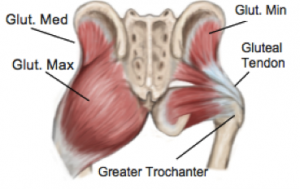
The gluteal muscles are three large muscles located at the back of the pelvis that provide most of the muscle bulk of the buttock region. These muscles work together to keep your pelvis level when standing and are responsible for many movements of the hip. They play an important role in standing, walking and running.
The two deepest gluteal muscles, gluteus medius and gluteus minimus, attach from the center of the pelvis (the sacrum) and insert into the bony outer region of the upper thigh, called the greater trochanter via the gluteal tendons.
What causes tendons to develop tendinopathy?
Tendons, like muscles, skin and bones are living tissues and their strength and elasticity is influenced by a variety of factors, including hormones, age, how often and how much they are used. Rapid changes in activity levels or simply performing the same tasks too often can place a tendon under more stress than it can tolerate and it begins to break town.
Recently it has been shown that tendon health is also negatively affected by compressive forces, which can occur from blunt trauma or even habits such as crossing the legs, or sleeping on your side on a hard mattress.
What are the symptoms of Gluteal Tendinopathy?
When gluteal tendons are affected by tendinopathy, a typical pattern of sharp pain at the outside of the hip with specific movements is present. The pain is usually worse with walking, going up and down stairs and running. The pain can become quite severe, and eventually can impact day-to-day activities.
How can physiotherapy help?
A thorough assessment is required for an accurate diagnosis and once gluteal tendinopathy is confirmed, your physiotherapist will be able to identify which factors have contributed to your condition and help to address these. It has been shown that specific loading exercises and muscular retraining can stimulate the tendon to heal and remodel the collagen fibers into a more organised pattern again. Your physiotherapist can investigate any postural habits or activities that are contributing and address these as required.
None of the information in this blog is a replacement for proper medical advice. Always see a medical professional for advice on your individual injury.